betaLiver Function Blood Test Interpreter
Fatty liver
Enter values to interpret
Liver scarring
Enter values to interpret
AST: 000 IU/L
ALT: 000 IU/L
ALP: 000 IU/L
Why this beats ChatGPT
All research is done by humans. AI was only used to refine the writing for better readability.
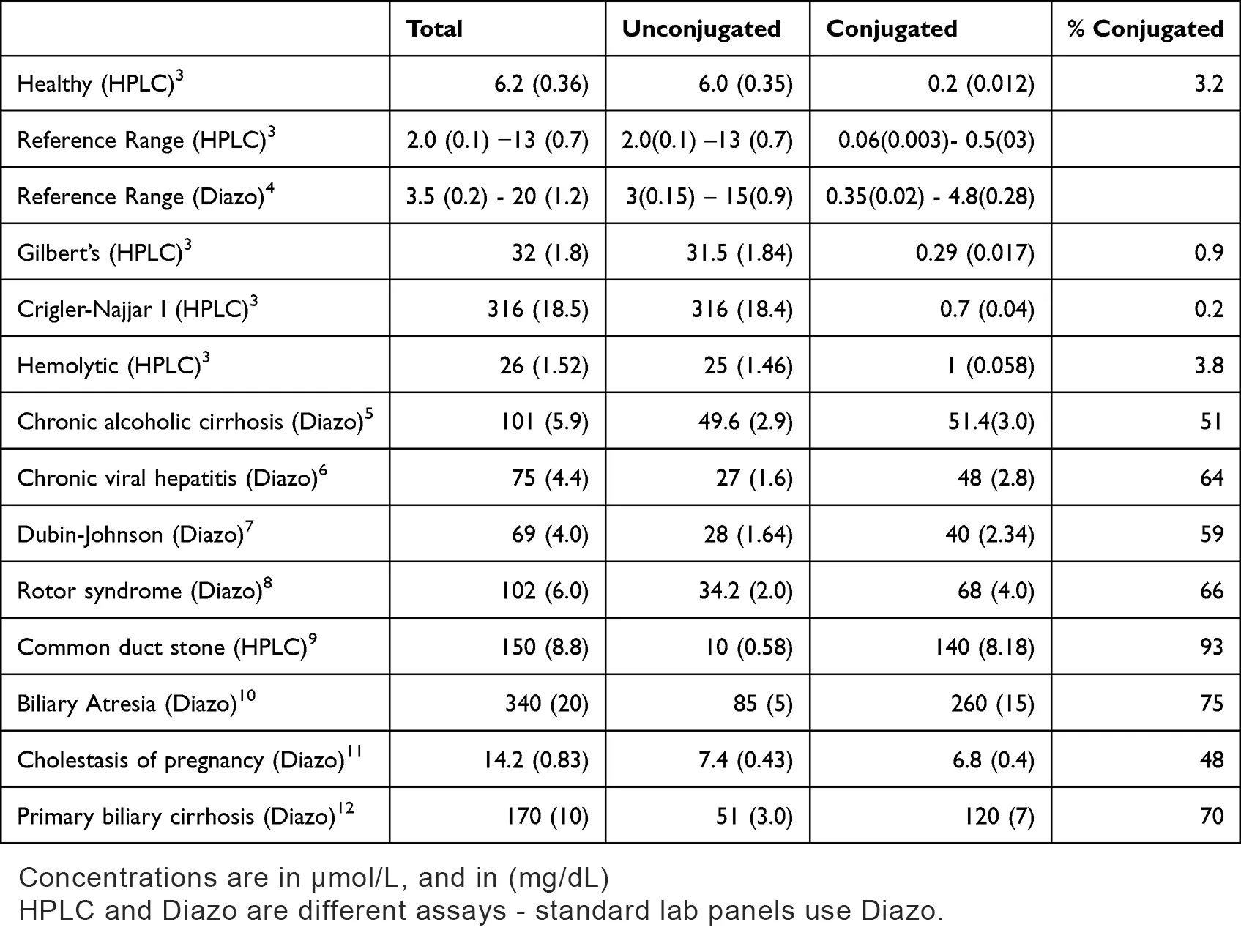
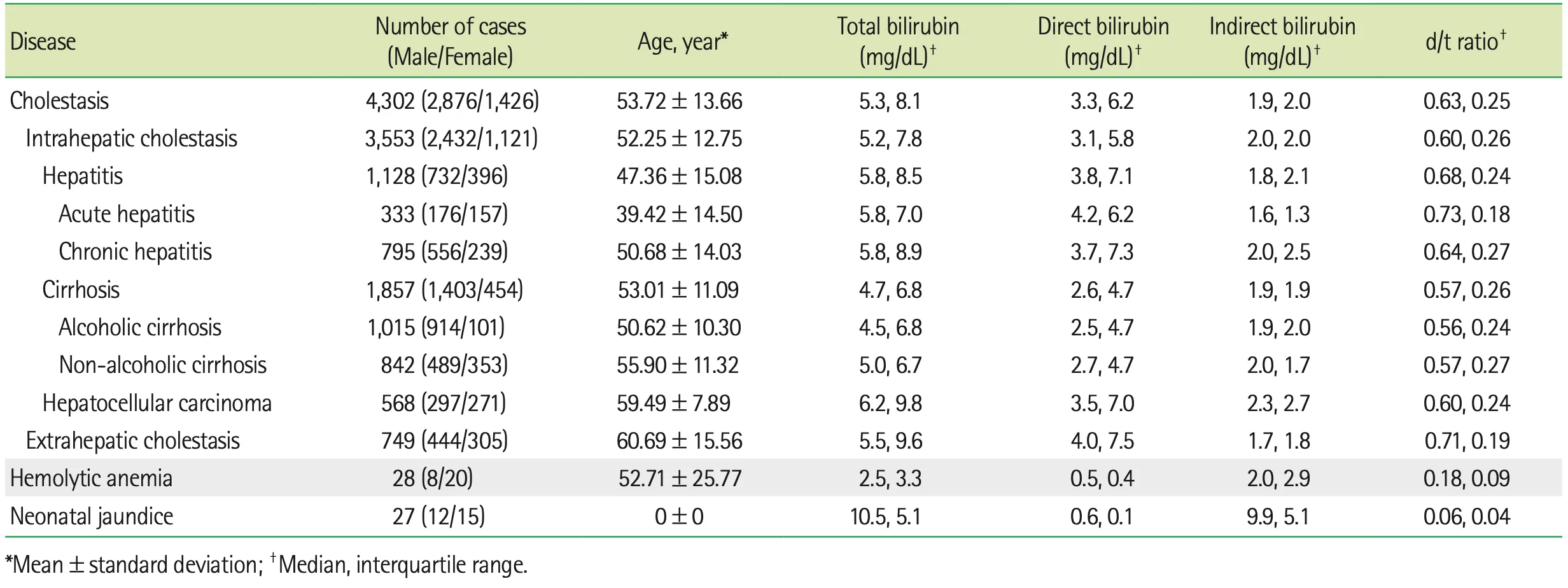
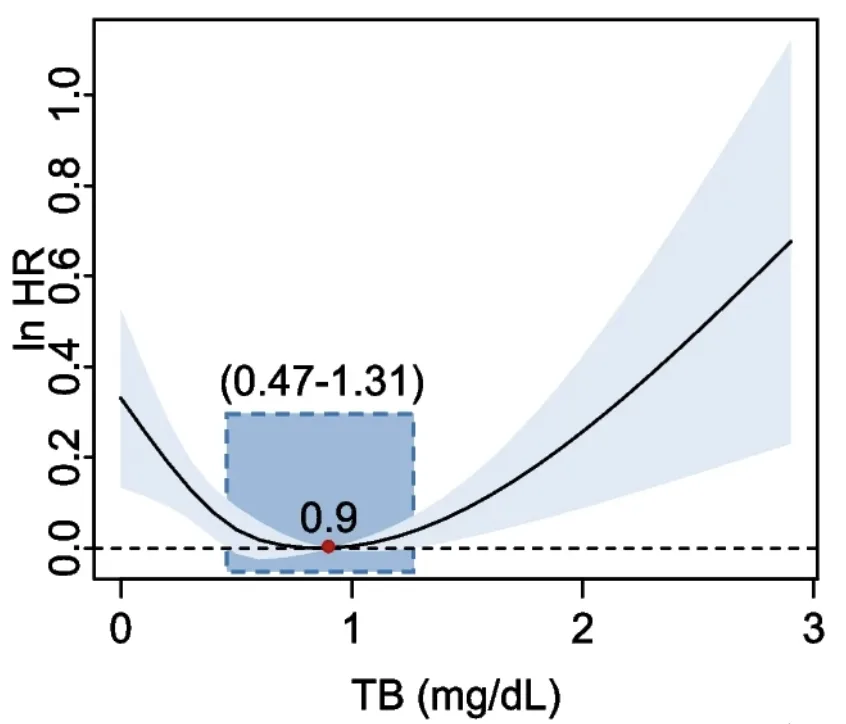
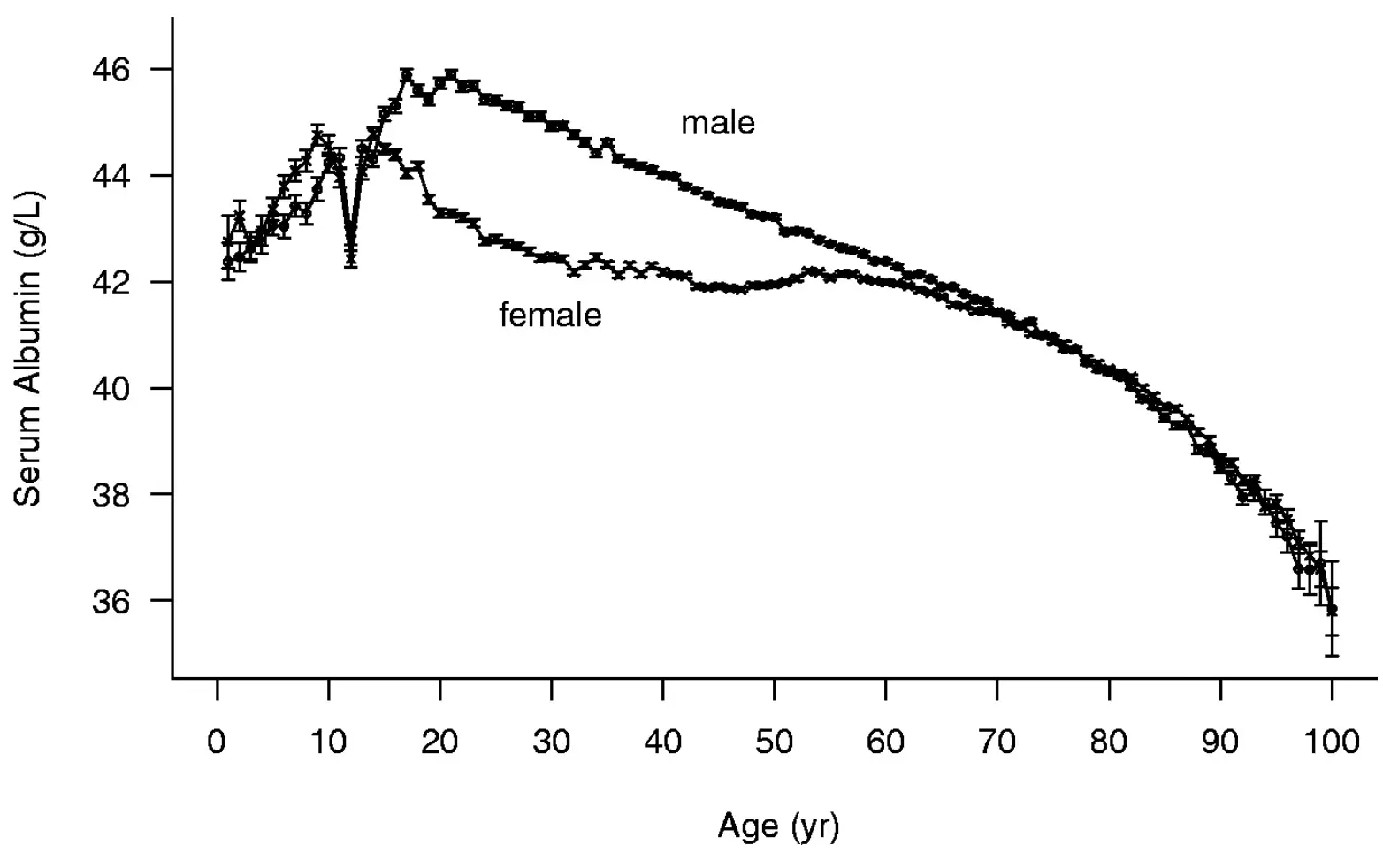
Optimal ranges, not just “normal”
Generic AI uses normal lab ranges (based on population averages). This tool uses functional, best-outcome targets.
Evidence-locked math. Not hallucinations
Generic AI chatbots don’t know which calculated indices are best or their optimal cutoff values.
Clinically significant differentials
We run relevant differential diagnosis calculations, but only when it's clinically significant.
Privacy by default
Everything happens in your browser and no personal or medical information leaves your computer.
Special Thanks to the Following Researchers and Doctors
I extend my gratitude for their invaluable consultation during the development of this Liver Function Blood Test Interpreter tool.
Kazuya Kariyama, M.D., Ph.D.
Deputy Hospital Director at Okayama City Hospital, Department of Gastroenterology.
Dr. Kariyama is the inventor of the FIB-3 index and provided valuable insights into its cut-off values and clinical application.
Prof. Hongbing Sun, Ph.D.
Department of Chemistry, Biochemistry, and Physics, Rider University.
Prof. Sun is the inventor of the LSS index and contributed valuable insights into its calculation, interpretation, and optimal cut-off values.
Dr. Luis E. Simental Mendía, Ph.D.
Biomedical Research Unit, Mexican Institute of Social Security.
Dr. Simental's research focuses on obesity-related metabolic disorders. He is the inventor of the TyG index and provided expert consultation on its calculation and application.
About the site author
My personal mission is to extend human lifespan by collectively adding 1 million years to people's lives.
That’s why I made this site 100% free—no sign-up, no email. Just instant results.
Zsolt SzaboPrecision Health Consultant for Longevity Clinics, Biohacker, and Software Engineer